The Metaverse in Digital Health

Metaverse is the augmented virtual world formed by the convergence of virtual and physical space. Users interact within this created world, meeting each other virtually, and immersing themselves in performing virtual activities, that could later lead to real experiences. There are advantages, disadvantages, limitations, and challenges in the actual deployment of the Metaverse.
Directly interacting with digital products and solutions will be a new experience for the healthcare provider and the beneficiary. Proof that deploying the metaverse will lead to improvement in health care outcomes will lead to the development of a business model, insurance reimbursement, and behavioral modification necessary for accepting and using, a hitherto unused method in patient care.
The Greek word Meta (μετα) implies “with, among, after, beyond, that is transcending reality”, as in the term metaphysics. Augmented Reality (AR) / Virtual Reality (VR), Extended Reality (XVR) Mixed Reality (MR), Internet of Medical Things (IoMT), Web 3.0, I Cloud, EDGE (Enhanced Data for Global Evolution), Quantum and Spatial Computing, Robotics, AI, 5G and Blockchain when deployed individually or collectively for one or more applications result in the Metaverse. Metaverse is the interface where users are immersed in a make-believe world with visual, auditory, and even sensory inputs.
Currently, the FDA reviews VR/AR devices through its Medical Extended Reality Program, a precursor to setting regulatory requirements for future devices and uses. Protecting virtual patients from bad care, predatory schemes, false claims, and fraud must be a priority.
Individuals will face a reality, without physically experiencing the reality. In the last 22 years from the Web of Science database alone, 34,000 papers relating to the Health Metaverse were identified.
Modeling the physical world digitally enables tracking and tracing healthcare facilities, equipment, and supplies in near-real-time, matching supply and demand. Virtual models are made of supply chains, facilities, and human organs.
In two decades, digital twins will be commonplace. Every single bit of health data from in utero to even cryofreezing of organs after clinical death, will be perpetually stored in the cloud. Wearable devices will converge, storing terabytes of individual information.
Immersive learning outside the OT is valuable. Head-mounted displays (HMDs) contribute to surgical accuracy and education. Surgical procedures are simulated enabling practice on a hologram on a virtual patient.
AR provides real-time guidance in the field of view, through integration with surgical navigation systems and data fusion from multiple imaging sources. With interoperability being crucial, assets such as avatars, 3D models, MR, spatial settings, and data must work across all platforms and networks. VR/AR goggles, hand controllers, headgear and even a full-body haptic suit to interact with healthcare providers in a virtual space may be necessary. Students wearing VR headsets practice lifesaving cardiac procedures on life-like mannequins simulating various cardiac diseases.
Digital Twin is a highly complex virtual model of a counterpart (the twin) of a physical thing. The ‘thing’ could be a car, a building, a bridge, a jet engine, or a human. Connected with sensors on the physical asset, collected data is mapped onto the virtual model. The Digital Twin of a patient is created by transferring the patient’s genomic and clinical data and real-time changes in body parameters to the digital environment. The Digital Twin is the virtual twin of an individual - a 1:1 copy of all health data from antenatal to clinical death. Digital twins are the foundations of the metaverse.
When one falls ill, the “virtual profile” would be computationally treated. Philips and Siemens have developed digital twins of the human heart, to simulate cardiac catheter interventions. Sim & Size platform helps neurosurgeons treat aneurysms with personalized simulations. Digital Twin-based Indian startups are deploying the ‘Whole Body Digital Twin’ to assist individuals prevent and reverse chronic metabolic diseases.
Virtual Reality technologies are being introduced in healthcare. A recent report identified 12,000 publications on VR applications in healthcare. VR is an immersive, completely artificial, computer-simulated image and environment with real-time interaction stimulating all senses. VR training with HMD provides an immersive and interactive learning environment.
Problems and Challenges: Evidence that investment in the Metaverse is cost-effective, appropriate, need-based, and will improve healthcare outcomes is awaited. Interoperability, portability, stakeholder customization, human factors (skills, resistance, distrust, cyber-attacks), legislation, and regulation need to be addressed. Digital Health has products and solutions that give patients and providers the ability to view, share, exchange, create, and interact with digital content. For a Health Metaverse, the ecosystem requires a profound digital transformation in process, workflow, practice, and delivery methods. The Metaverse needs to share data across institutional, systematic, and national lines. It is also prone to cyber-attacks, a risk, that VR organizations need to assess. Privacy and compliance issues are also a challenge.
Economic Impact of the Health Metaverse: When Mark Zuckerberg rechristened Facebook into META and diverted $10 billion into the Metaverse division he was getting future-ready. AR alone in global healthcare is expected to be $4.15 billion by 2025.
Conclusion
The metaverse though in its infancy has promise for healthcare innovation and improvement. Having a place where people can face reality without necessarily experiencing reality is intriguing as is watching the implementation evolve. No wonder the metaverse is being described as one of the best innovations in healthcare in recent years.
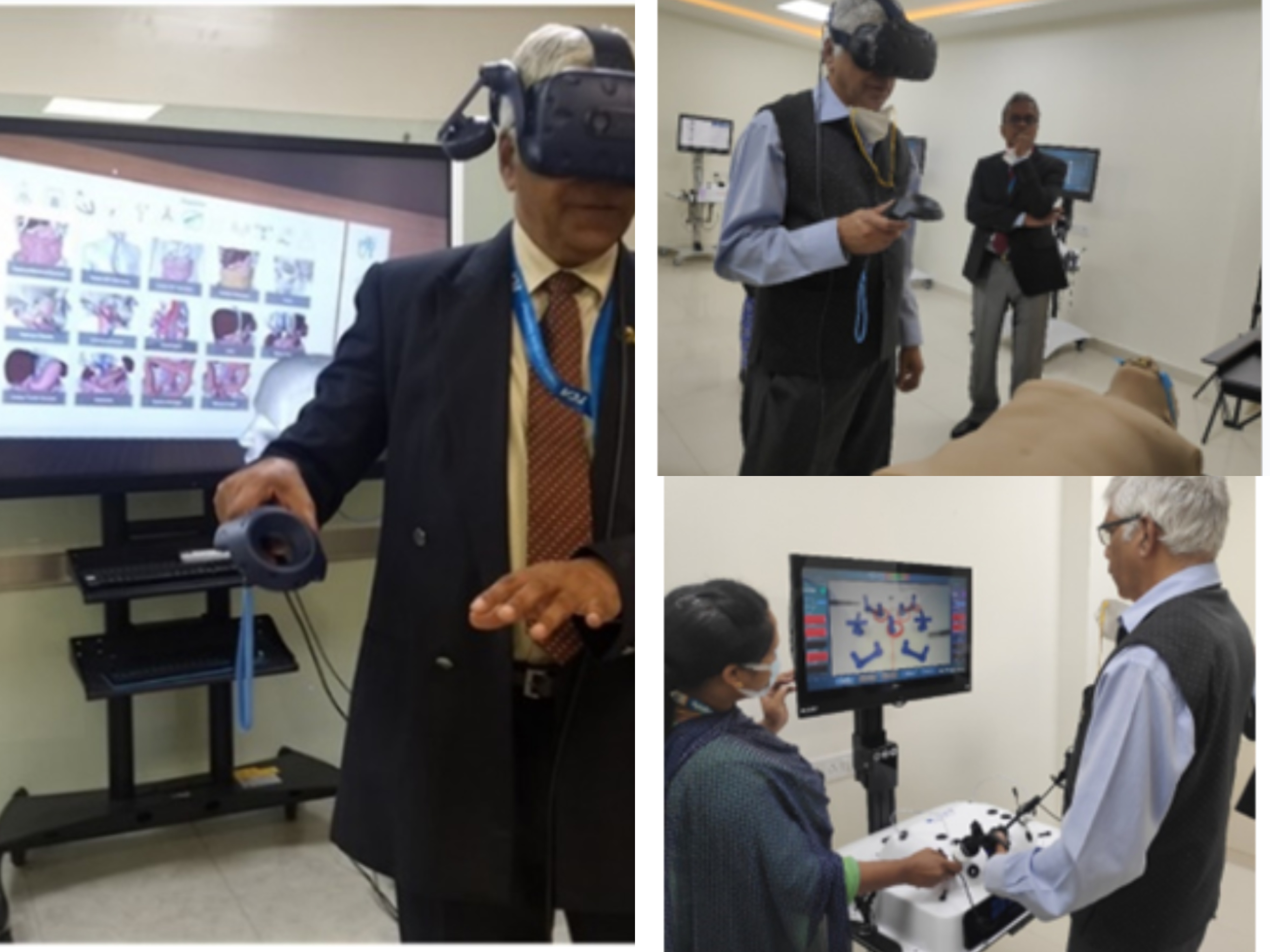
The Author in a Virtual World in an Advanced Simulation Center
Stay tuned for more such updates on Digital Health News